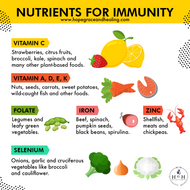
Nutrients for Immunity and How They Act Topically in Skin Care Products - Part I
Posted by T. Schuur | Integrative Health Practitioner | Aromatherapist | Herbalist | Botanical Chemistry & Formulation on 7th Jul 2020

Vitamin C:
The antioxidant properties of vitamin C (ascorbic acid) and its role in collagen synthesis make vitamin C a vital molecule for skin health. Dietary and topical ascorbic acid have beneficial effects on skin cells, and some studies have shown that vitamin C may help prevent and treat ultraviolet (UV)-induced photodamage.
Topically. ascorbic acid has important physiological effects on skin: inhibiting melanogenesis, promoting collagen biosynthesis and preventing free radical fonnation. These effects are all closely related to the well-known antioxidant properties of this compound. L-Ascorbic acid also inhibits NFkB, which s responsible for the activation of different pro-inflammatory cytokines such as IL-I, IL-6 and IL-8. Therefore, ascorbic acid has potential anti-inflammatory activity and can be used to treat skin conditions such as acne vulgaris and rosacea. It also can promote wound healing and prevent post-inflammatory hyperpigmentation.
Applying antioxidants topically is an efficient way to increase skin levels, to help protect against reactive oxygen species (ROS) and combat cutaneous damage.
Vitamin C can be provided to the skin through topical application. The stratum corneum is the primary obstacle to efficient vitamin C absorption from external sources1 removal of the stratum corneum by laser, chemical, or mechanical methods enhances absorption2. Although similar studies are still required for humans, studies in laboratory animals show that percutaneous vitamin C absorption greatly depends on pH. Preparations with a pH below 4.0 aid in transport by promoting the uncharged form of vitamin C, ascorbic acid1. Although concentrations of vitamin C up to 30% have been used for animal studies, maximal absorption was achieved with a 20% vitamin C solution, with higher concentrations showing lower absorption1. Topical application of ascorbic acid will cross the epidermis into the underlying dermal layers.
Human studies with subjects using topically applied solutions of 0.6%-10.0% vitamin C or its synthetic derivatives have not reported adverse effects3, 4-12.

Vitamin A:
The term “retinoids” refers to vitamin A and the various compounds derived from vitamin A. Skin is a major retinoid-responsive tissue.
Cells in both the epidermis and dermis contain proteins and receptors that mediate the biological effects of vitamin A metabolites in the skin.
A commonly experienced side effect following topical application of retinoids is "retinoid dermatitis." Adjusting the dose and frequency of retinoid application can reduce adverse skin reactions.
Topical retinoids have a well-documented effect on skin health, with the majority of clinical evidence relating to their treatment of acne vulgaris and certain signs of photoaging.
Pretreatment with topical retinoids can mitigate some of the ultraviolet radiation (UVR)-induced changes that damage dermal collagen.
Topical retinoids induce clinical improvements in photoaged skin, including a reduction in fine wrinkling, increased smoothness, and diminished hyperpigmentation.
The longevity of topical retinoid effects is uncertain, and a long-term maintenance regimen is necessary in order to sustain retinoid-induced clinical improvements.
Studies in animals demonstrate that vitamin A mitigates cortisone-induced defects in wound healing.
Topical tretinoin is considered a very safe and effective treatment for mild to moderate acne, while oral isotretinoin is used to treat severe cases of acne that are resistant to topical therapies.
A very common side effect of topical retinoid therapy is "retinoid dermatitis," also referred to as retinoid irritation or retinoid reaction. Retinoid dermatitis is characterized by erythema, scaling, dryness, and pruritis13-15. Topical retinoids induce changes in the epidermis that lead to increased proliferation and altered differentiation of keratinocytes (see Photoaging); this in turn disrupts the barrier of the skin and contributes to the features of retinoid dermatitis (personal communication, Dr. Gary Fisher, December 2012). The level of irritation correlates with the potency of the applied vitamin A metabolite. Thus, adjusting the timing, dose, and form of topical retinoid can influence the retinoid reaction. For example, 0.025% topical tretinoin has the same effect as 0.05% tretinoin on fine wrinkles and roughness, but with less irritation and after a longer exposure time14. Notably, tretinoin concentrations less than 0.01% are largely ineffective in the treatment of photodamaged skin16-18. Topical application of other retinoids, such as isotretinoin and retinol also lead to clinical improvements, again with less skin irritation and after a much longer exposure time than tretinoin19.
Percutaneous absorption of topical retinoids is minimal, thus very little of the active ingredient reaches the systemic circulation. Repeated application of 2 g of 0.025% tretinoin gel (equivalent to 0.05 mg at-RA) to the face, neck, and upper part of the chest nightly for 14 days did not influence the concentration of plasma at-RA and its metabolites in a small sampling of human volunteers (N=4)20. In another study, radiolabeled tretinoin (0.05%) in cream or emollient was applied to facial skin, and the amount of tretinoin reaching the circulation was measured after single or repeated (once daily for 28 days) application21. In both cases, no significant changes in plasma tretinoin concentration were observed. Additionally, only 1-2% of the radiolabeled-tretinoin dose was excreted in the urine and feces, indicating that very low levels of topical tretinoin reach the systemic circulation.

Vitamin D:
Healthy vitamin D levels might help prevent skin from prematurely aging but too much sun leads to accelerated skin aging. Some studies have found that vitamin D can help treat skin conditions like dry skin, psoriasis, or eczema.
Sunlight exposure is the primary source of vitamin D for most people. Solar ultraviolet-B radiation (UVB; wavelengths of 290 to 315 nanometers) stimulates the production of vitamin D3 from 7-dehydrocholesterol (7-DHC) in the epidermis of the skin (see Production in Skin)22. Hence, vitamin D is actually more like a hormone than a vitamin, a substance that is required from the diet. Vitamin D3 enters the circulation and is transported to the liver, where it is hydroxylated to form 25-hydroxyvitamin D3 (calcidiol; the major circulating form of vitamin D). In the kidneys, the 25-hydroxyvitamin D3-1-hydroxylase enzyme catalyzes a second hydroxylation of 25-hydroxyvitamin D, resulting in the formation of 1,25-dihydroxyvitamin D3 (calcitriol, 1α,25-dihydroxyvitamin D] — the most potent form of vitamin D23. Most of the physiological effects of vitamin D in the body are related to the activity of 1,25-dihydroxyvitamin D3; see the article on Vitamin D. Keratinocytes in the epidermis possess hydroxylase enzymes that locally convert vitamin D to 1,25-dihydroxyvitamin D324-26,the form that regulates epidermal proliferation and differentiation (see Metabolism in keratinocytes).
Topical application
Calcitriol (1,25-dihydroxyvitamin D3) has been used topically to treat certain skin conditions, including psoriasis, a skin condition that involves a hyperproliferation of keratinocytes. Several studies found that topical use of calcitriol (3 μg/g) ointment is safe and may be an effective treatment for plaque-type psoriasis27-29.The vitamin D analog called calcipotriene or calcipotriol has also been used as a treatment for chronic plaque psoriasis, either alone or in combination with corticosteroids30-31.

Vitamin E:
Vitamin E is a powerful antioxidant that may be effective at reducing UV damage in skin. And vitamin E applied topically may help nourish and protect your skin from damage caused by free radicals.
Topical application of vitamin E has been used in a wide variety of forms throughout history, ranging from the application of oils to the skin surface to the use of modern cosmetic formulations. Just as sebum provides a delivery mechanism for vitamin E to the stratum corneum, topical applications of vitamin E permeate the epidermis and dermis32-33. The rate of percutaneous vitamin E absorption and factors that influence its penetration are largely unknown in humans, with a large range of concentrations and times used in various studies. It is generally assumed that solutions with vitamin E concentrations as low as 0.1% can increase vitamin E levels in the skin34. Interestingly, vitamin E levels in the dermis increase greatly after topical application, likely accumulating in the sebaceous glands39. However, although it is increased after topical delivery, the concentration of vitamin E in the dermis is lower than in the stratum corneum. Skin supplied only with dietary vitamin E primarily contains α- and γ-tocopherol35-37; by contrast, skin supplied with synthetic vitamin E topically can contain a mixture of different tocopherols and/or tocotrienols38-39. In terms of penetration and absorption following topical application, tocotrienols and tocopherols accumulate in skin at varying rates, but the mechanisms governing these differences are unclear33.
After topical application, vitamin E accumulates not only in cell membranes but also in the extracellular lipid matrix of the stratum corneum, where vitamin E contributes to antioxidant defenses. However, much of a topically applied dose of vitamin E alone will be destroyed in the skin following exposure to UV light38. This suggests that although vitamin E is working as an antioxidant, it is unstable on its own and easily lost from the skin. Thus, improving the stability of topical applications with vitamin E is important. Products containing both vitamin C and vitamin E have shown greater efficacy in photoprotection than either antioxidant alone (see Photoprotection).
The stability of topical vitamin E solutions may also be increased by the use of vitamin E conjugates. These vitamin E derivatives are usually commercially produced esters of tocopherol (although tocotrienol esters have been formulated) that are resistant to oxidation but can still penetrate the skin layers. Vitamin E conjugates, however, do not have antioxidant functions. To be effective, the molecule conjugated to vitamin E must be removed by enzymes within a cell. Since the stratum corneum contains metabolically inactive cells and the remaining layers of the epidermis and dermis may contain a large volume of extracellular proteins, it is unclear how efficiently ester conjugates are converted to “free” vitamin E in skin. Depending on the compound and the model system used, the effectiveness of these formulations can vary greatly40-44, and studies often do not compare the application of vitamin E conjugates to the application of unmodified vitamin E molecules.
Because vitamin E can absorb UV light to produce free radicals (see Photoprotection), there is the possibility that heavy sunlight exposure after topical application can cause skin reactions. However, concentrations of vitamin E between 0.1%-1.0% are generally considered safe and effective to increase vitamin E levels in the skin, but higher levels of α-tocopherol have been used with no apparent side effects40. On the other hand, studies of dose-dependent vitamin E accumulation and effectiveness in skin protection are lacking. Some forms of vitamin E, especially ester conjugates, have led to adverse reactions in the skin, including allergic contact dermatitis and erythema. Although such reactions may be due to oxidation by-products, the emulsion creams used for topical delivery of compounds may also contribute to the observed effects45.